Hand Hygiene Competency

Hand Hygiene Competency
Hand Hygiene May Stop Health Care Associated Infections (HCAI)
Health care-associated infections (HCAI) are also referred to as “nosocomial” or “hospital” infections. They are defined as follows:
“An infection occurring in a patient during the process of care in a hospital or other health-care facility which was not present or incubating at the time of admission. This includes infections acquired in the health-care facility but appearing after discharge and also occupational infections among health-care workers of the facility.”
What is hand hygiene?
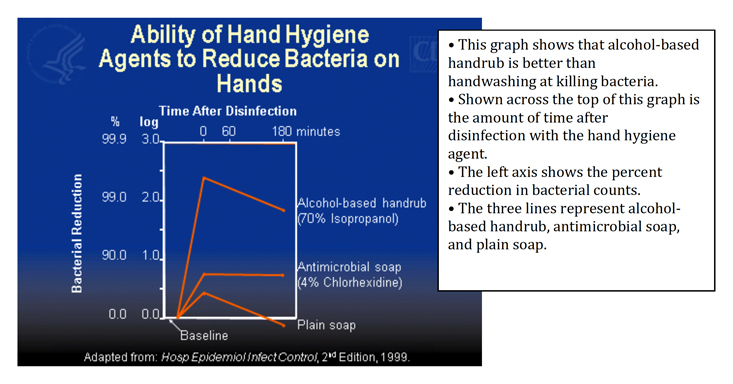
Hand hygiene is the action of cleaning hands. There are two ways to clean hands. Using an alcohol based hand rub, which kills organisms in seconds or, when hands are visibly soiled, using soap and running water.
Hand Rubbing Procedure: RUB HANDS FOR HAND HYGIENE! WASH HANDS WHEN VISIBLY SOILED Duration of the entire procedure 20-30 seconds
- Apply a palmful of the product in a cupped hand, covering all surfaces;
- Rub hands palm to palm;
- Right palm over left dorsum with interlaced fingers and vice versa;
- Palm to palm with fingers interlaced;
- Backs of fingers to opposing palms with fingers interlocked;
- Rotational rubbing of left thumb clasped in right palm and vice versa;
- Rotational rubbing, backwards and forwards with clasped fingers of right hand in left palm and vice versa;
- Once dry, your hands are safe.
Hand Washing Procedure: HANDS WHEN VISIBLY SOILED! OTHERWISE, USE HANDRUB
Duration of the entire procedure: 40-60 seconds
- Rub hands palm to palm;
- Apply enough soap to cover all hand surfaces;
- Wet hands with water;
- Right palm over left dorsum with interlaced fingers and vice versa;
- Palm to palm with fingers interlaced;
- Backs of fingers to opposing palms with fingers interlocked;
- Rotational rubbing of left thumb clasped in right palm and vice versa;
- Rotational rubbing, backwards and forwards with clasped fingers of right hand in left palm and vice versa;
- Rinse hands with water; Your hands are now safe.
- Use towel to turn off faucet; Dry hands thoroughly with a single use towel.
HCAI Burden... In the United States
- In modern health-care facilities in the developed world: 5–10% of patients acquire one or more infections
- In intensive care units, HCAI affects about 30% of patients and the attributable mortality may reach 44%
- Incidence: 5–6%; 1.7 million affected patients
- Urinary Tract Infection: 36%; 561,667 episodes, 13,088 deaths
- Surgical Site Infection: 20%; 274,098 episodes (1.98%)
- Catheter Related Bloodstream Infections: 11%; 250,000 episodes, 28,000 deaths
- Ventilator Associated Pneumonia: 11%; 5.4/1000 ventilator-days
- Attributable mortality: 3.6%, approximately 99,000 deaths
- Annual economic impact: about $4.5 billion
Transmission: Transmission of health care-associated pathogens from one patient to another via health-care workers' hands requires 5 sequential steps. “80% of all infectious diseases are transmitted by touch.”
Germs are present on patient skin and surfaces in the patient surroundings
By direct and indirect contact, patient germs contaminate health-care workers' hands
Germs survive and multiply on health-care workers' hands
Defective hand cleansing results in hands remaining contaminated
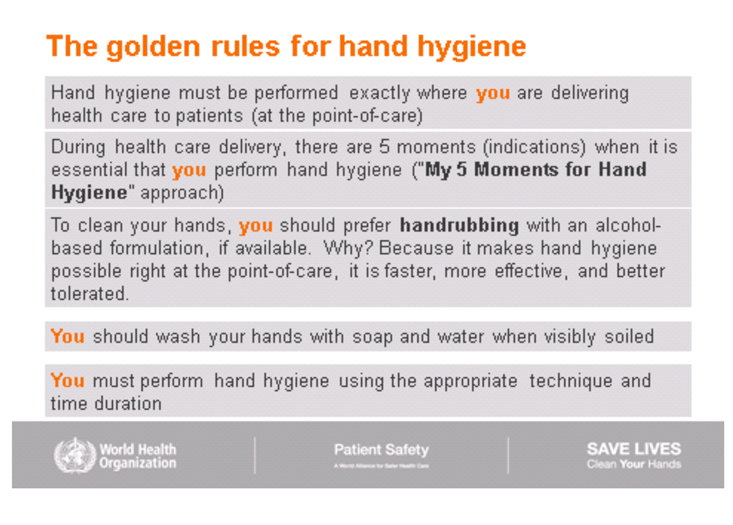
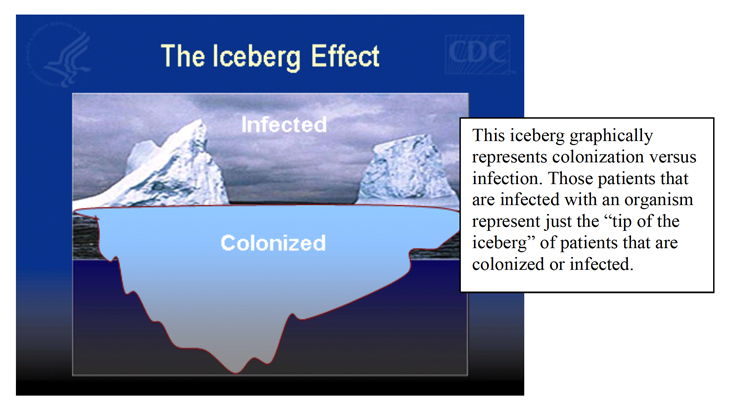
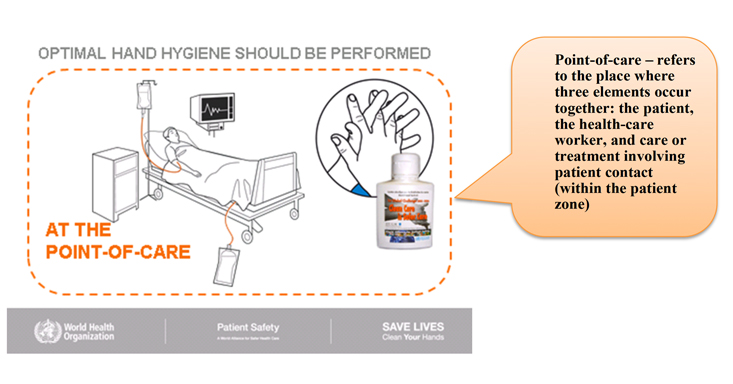
Transfer of pathogens from one source to another. Handwashing agents cause irritation and dryness Use of alcohol based hand rubs decrease the likelihood of drying or irritating the skin Sinks are inconveniently located/lack of sinks Use of alcohol based hand rubs are to be used at the point of care, no need to use a sink for routine hand hygiene, only needed when visibly soiled or when coming into contact with bodily fluids. Lack of soap and paper towels Only needed as stated above, use of alcohol based rubs are more effective in killing pathogens. Too busy/insufficient time The time saved by using hand rubs instead of handwashing can save a nurse up to 1 hour daily. Patient needs take priority Yes they do, but proper hand hygiene and good patient care do not need to be mutually exclusive. Low risk of acquiring infection from patients The risk is always there. By using proper standard precautions and hand hygiene the risk can be cut substantially. But also remember the risk we may cause to the client. They are the ones with the multiple ports of entry and compromised conditions. There are 5 essential moments where the healthcare worker is to use hand hygiene. Following are those 5 moments, the rationale and examples of each. BEFORE TOUCHING A PATIENT: To protect the patient against harmful germs carried on your haps BEFORE PERFORMING A CLEAN OR ASEPTIC PROCEDURE -To protect the patient against harmful germs, including the patient's own, from entering his/her bodp AFTER BODY FLUID EXPOSURE RISK - To protect yourself and the health-care environment from harmful patient germs. AFTER TOUCHING A PATIENT – To protect yourself and the health-care environment from harmful patient germs. AFTER TOUCHING A PATIENT'S SURROUNDINGS –To protect yourself and the health-care environment from harmful patient germs.
“But my patient isn't infected!”
So Why All the Fuss About Hand Hygiene?
Self-Reported Factors for Poor Adherence with Hand Hygiene
Barrier
Solution
Consider:
Average time usually adopted by health-care workers: <10 seconds
Based on seven (60 second) handwashing episodes per hour
Based on seven (20 second) handrub episodes per hour
THE 5 ESSENTIAL MOMENTS
HAND HYGIENE AND MEDICAL GLOVE USE
- The use of gloves does not replace the need for cleaning your hands.
- Hand hygiene must be performed when appropriate regardless of the indications for glove use.
- Remove gloves to perform hand hygiene, when an indication occurs while wearing gloves.
- Discard gloves after each task and clean your hands – gloves may carry germs.
- Wear gloves only when indicated according to Standard and Contact Precautions (see examples in the pyramid below) – otherwise they become a major risk for germ transmission.
The Glove Pyramid- Used to aid decision making on when to wear (and not wear) gloves
Gloves must be worn according to STANDARD and CONTACT PRECAUTIONS The pyramid details some clinical examples in which gloves are not indicated, and others in which clean or sterile gloves are indicated. Hand hygiene should be performed when appropriate regardless of indications for glove use
STERILE GLOVES INDICATED
Any surgical procedure; vaginal delivery; invasive radiological procedures; performing vascular access and procedures (central lines); preparing total parental nutrition and chemotherapeutic agents.
EXAMINATION GLOVES INDICATED IN CLINICAL SITUATIONS
Potential for touching blood, body fluids, secretions, excretions and items visibly soiled by body fluids.
DIRECT PATIENT EXPOSURE: Contact with blood; contact with mucous membrane and with non-intact skin; potential presence of highly infectious and dangerous organism; epidemic or emergency situations; IV insertion and removal; drawing blood; discontinuation of venous line; pelvic and vaginal examination; suctioning of tracheal tubes.
INDIRECT PATIENT EXPOSURE: Emptying emesis basins; handling/cleaning instruments; handling waste; cleaning up spills of body fluids.
GLOVES NOT INDICATED (except for CONTACT precautions)
No potential for exposure to blood or body fluids, or contaminated environment
DIRECT PATIENT EXPOSURE: Taking blood pressure, temperature and pulse; bathing and dressing the patient; transporting patient; caring for eyes and ears (without secretions); any vascular line manipulation in absence of blood leakage.
INDIRECT PATIENT EXPOSURE: Using the telephone; writing in the patient chart; giving oral medications; distributing or collecting patient dietary trays; removing and replacing linen for patient bed; placing non-invasive ventilation equipment and oxygen cannula; moving patient furniture.
- Jay Hardy. CLS, SM (ASCP) 11 Handwashing Facts
- CDC
- WHO
- RMIT University
- WebMD

call for support
(630) 236-3501Email Us
[email protected]Available Time
8 A.M - 4:30 P.M. (Mon–Fri)Copyright © 2025 - American Home Health Care. All right reserved.
Powered By: Aguilera Web Design